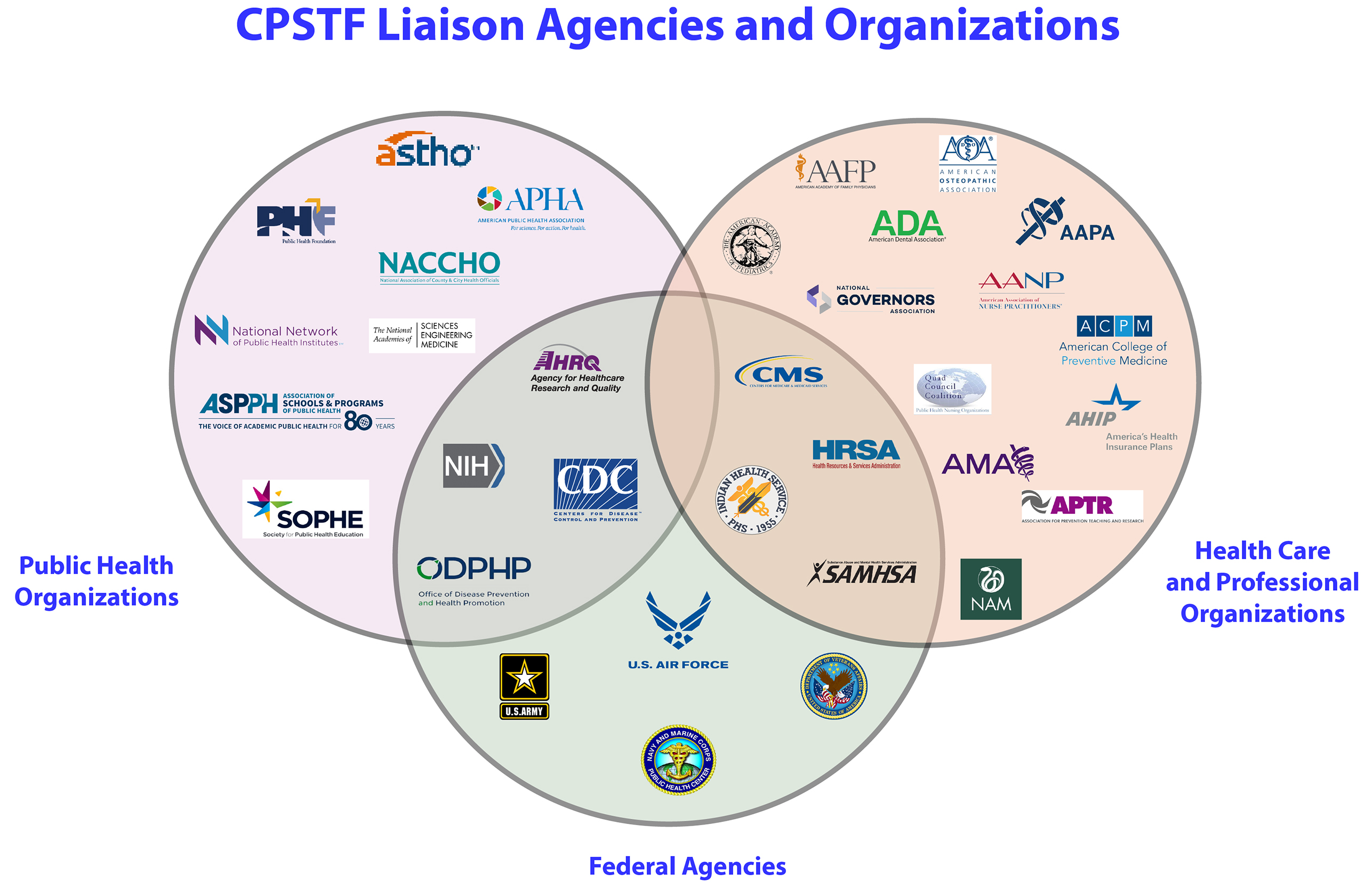
Liaisons to the Community Preventive Services Task Force
CPSTF engages with 32 agencies and organizations invited to serve as Liaisons. They support the work of the task force and contribute to The Community Guide by:
- Promoting the value and use of The Community Guide in their agencies or organizations
- Representing the views, concerns, and needs of their organization and constituents
- Participating in the selection and prioritization of CPSTF topics
- Engaging in systematic reviews of interventions
- Disseminating CPSTF recommendations and findings
- Translating CPSTF recommendations into practice
- Providing feedback on how well CPSTF recommendations meet the needs of their constituents